A few weeks ago I had my last day as a CNA in a convalescent home. In no way did I anticipate what an emotional experience that would be. My almost two years in that position were, without a doubt, the hardest thing I’ve ever done. I was hit, scratched, spat on, cursed and yelled at, vomited on, had urine splash on my face–and once had projectile, bloody diarrhea hit my face. Fortunately the communicable diseases spared me.
I’ve cared for people who weigh over 300 lbs., have C. diff, and have no ability roll over. let alone stand up. This means that the CNA needs to roll their body over for diaper changes, which are frequent with C. diff. Some patients don’t want their nasty, soiled, diaper changed, and push back on the wall as hard as they can while you try to push back with one hand and position the clean diaper with the other. I worked in a “no lift” facility but everyday lifted several people from the bed to the wheelchair. Yes, I’m massaging my own back right now.

Most of the patients were really wonderful–being old can make one aware of their own vulnerabilities, and very tender and appreciative. But sometimes it’s the opposite, and some are struggling with serious issues. Imagine being an older woman with Alzheimer’s, in a nursing home, with no family visiting ever. I can’t imagine how vulnerable that would feel (and hope I never do).
Unlike the hospital, in a convalescent home the CNA spends more time with the patients/residents than anyone else on staff. The care in this setting is generally not urgent–for the most part the patients require help with bathing, toileting, dressing, and sometimes feeding. Because of the longer length of residency, CNAs get to know patients pretty well and are also responsible for reporting any changes in behavior–confusion, lethargy–and are usually the person present when things do become urgent, due to a fall, a stroke, or simply due to dire health that on a typial day is not quite bad enough to require hospital care.
RN and LVN positions have government imposed nurse/patient ratios, but that’s not the case for CNAs. It’s determined by the facility, and mine was about average–about eight patients during the day shift. It doesn’t sound like a lot–you might think “oh, eight patients, that gives you an hour with each person”. But we also pass breakfast and lunch trays, help feed some, change linens, take and record vital signs, and chart everything we do in the day for each person–did they eat, how much did they eat, are they self ambulatory in bed, out of bed, in the wheelchair, do they use a walker, do they need help getting dressed, how much help, did they have any snacks, how much, did they have any bowel movements or urinate, how many, at what time, was the stool hard, soft, or watery, do they have a catheter, how many cc’s of urine was collected, did they shower or sponge bath, how much help did you provide, did they leave the facility for any reason, were they turned and repositioned every two hours, etc. It’s A LOT of work.
I made $12 an hour, which was more than most of my co-workers. The health benefits, had I taken them, would have cost $900 a month for me and my family. We waived them and continued with our individually purchased plan, which was cheaper. My heart goes out to several co-workers who have worked that job for 10+ years, are wonderful, and such care for the residents as if they were their own family. They taught me so much, most importantly, what is true of every nursing job: that it simply is not ever, about you.
Tonight I start my first day on my own in my new position as a CNA in the Obstetrics unit, helping Mom’s with their new babies. 🙂
 gan necessary for survival—the brain, liver, kidneys (at least one), pancreas, and lungs come to mind–we still regard the heart as most integral to life, most likely because of its central location and role in pumping blood throughout our entire body.
gan necessary for survival—the brain, liver, kidneys (at least one), pancreas, and lungs come to mind–we still regard the heart as most integral to life, most likely because of its central location and role in pumping blood throughout our entire body.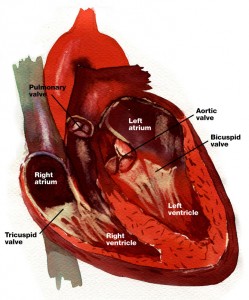 four chambers: two halves, with two chambers each—an atrium—some call it an auricle—and a ventricle. Each atria and ventricle pair pump blood to a different part of the body. The right half supplies the lungs with blood (via the pulmonary circuit), and the left half supplies the entire body and brain with blood (the systemic circuit). Because the left ventricle pumps blood to a much larger area than the right, it is larger and much more muscular than the right ventricle.
four chambers: two halves, with two chambers each—an atrium—some call it an auricle—and a ventricle. Each atria and ventricle pair pump blood to a different part of the body. The right half supplies the lungs with blood (via the pulmonary circuit), and the left half supplies the entire body and brain with blood (the systemic circuit). Because the left ventricle pumps blood to a much larger area than the right, it is larger and much more muscular than the right ventricle.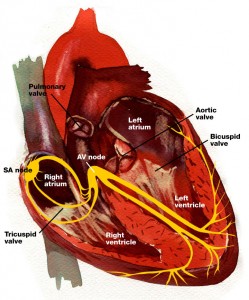 ginates, and it sets the pace for the electrical impulse as it travels to several other nodes and bundles of conducting fibers. It sets the pace for the heartbeat and can be sped up by the nervous systems if we experience a surge of epinephrine and the fight or flight urge. An ECG is measuring the electrical activity of the heart and can indicate damage to the SA node and the accompanying nodes and conducting neurons.
ginates, and it sets the pace for the electrical impulse as it travels to several other nodes and bundles of conducting fibers. It sets the pace for the heartbeat and can be sped up by the nervous systems if we experience a surge of epinephrine and the fight or flight urge. An ECG is measuring the electrical activity of the heart and can indicate damage to the SA node and the accompanying nodes and conducting neurons.